About ASD
Diagnosing autism spectrum disorder (ASD) can be difficult, since there is no medical test, like a blood test, to diagnose the disorders. Doctors look at the child’s behavior and development to make a diagnosis.
ASD can sometimes be detected at 18 months or younger. By age 2, a diagnosis by an experienced professional can be considered very reliable.[1] However, many children do not receive a final diagnosis until much older. This delay means that children with an ASD might not get the help they need.
Diagnosing an ASD takes two steps:
- Developmental Screening
- Comprehensive Diagnostic Evaluation
Developmental Screening
Developmental screening is a short test to tell if children are learning basic skills when they should, or if they might have delays. During developmental screening the doctor might ask the parent some questions or talk and play with the child during an exam to see how she learns, speaks, behaves, and moves. A delay in any of these areas could be a sign of a problem.
All children should be screened for developmental delays and disabilities during regular well-child doctor visits at:
- 9 months
- 18 months
- 24 or 30 months
- Additional screening might be needed if a child is at high risk for developmental problems due to preterm birth, low birth weight or other reasons.
- In addition, all children should be screened specifically for ASD during regular well-child doctor visits at:
- 18 months
- 24 months
- Additional screening might be needed if a child is at high risk for ASD (e.g., having a sister, brother or other family member with an ASD) or if behaviors sometimes associated with ASD are present
It is important for doctors to screen all children for developmental delays, but especially to monitor those who are at a higher risk for developmental problems due to preterm birth, low birth weight, or having a brother or sister with an ASD.
If your child’s doctor does not routinely check your child with this type of developmental screening test, ask that it be done.
If the doctor sees any signs of a problem, a comprehensive diagnostic evaluation is needed.
Comprehensive Diagnostic Evaluation
The second step of diagnosis is a comprehensive evaluation. This thorough review may include looking at the child’s behavior and development and interviewing the parents. It may also include a hearing and vision screening, genetic testing, neurological testing, and other medical testing.
In some cases, the primary care doctor might choose to refer the child and family to a specialist for further assessment and diagnosis. Specialists who can do this type of evaluation include:
- Developmental Pediatricians (doctors who have special training in child development and children with special needs)
- Child Neurologists (doctors who work on the brain, spine, and nerves)
- Child Psychologists or Psychiatrists (doctors who know about the human mind)
Some co-morbid disorders commonly seen among individuals with ASD include epilepsy, Tourette Syndrome, Attention Deficit Disorder, Obsessive Compulsive Disorder and Generalized Anxiety Disorder.
It is important the clinician assessing an individual for ASD also look at the possibility there are other co-occurring disorders.
Asperger syndrome (AS), also known as Asperger disorder (AD) or simply Asperger’s, is an autism spectrum disorder (ASD) that is characterized by significant difficulties in social interaction and nonverbal communication, alongside restricted and repetitive patterns of behavior and interests. It differs from other autism spectrum disorders by its relative preservation of linguistic and cognitive development. Although not required for diagnosis, physical clumsiness and atypical (peculiar, odd) use of language are frequently reported.
The syndrome is named after the Austrian pediatrician Hans Asperger who, in 1944, studied and described children in his practice who lacked nonverbal communication skills, demonstrated limited empathy with their peers, and were physically clumsy. The modern conception of Asperger syndrome came into existence in 1981 and went through a period of popularization becoming standardized as a diagnosis in the early 1990s. Many questions remain about aspects of the disorder. There is doubt about whether it is distinct from high-functioning autism (HFA);] partly because of this, its prevalence is not firmly established.] The diagnosis of Asperger’s was eliminated in the 2013 fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and replaced by a diagnosis of autism spectrum disorder on a severity scale.
Autism spectrum disorder (ASD) is characterized by:
- Persistent deficits in social communication and social interaction across multiple contexts;
- Restricted, repetitive patterns of behavior, interests, or activities;
- Symptoms must be present in the early developmental period (typically recognized in the first two years of life); and,
- Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
The term “spectrum” refers to the wide range of symptoms, skills, and levels of impairment or disability that children with ASD can have. Some children are mildly impaired by their symptoms, while others are severely disabled. The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) no longer includes Asperger’s syndrome; the characteristics of Asperger’s syndrome are included within the broader category of ASD.
PDD-NOS stands for pervasive developmental disorder not otherwise specified. In essence, it’s a diagnosis that means “on the autism spectrum, but not falling within any of the existing specific categories of autism.”
To explain more fully, there are five disorders that fall under the category of “pervasive developmental disorders” (PDDs). These include autism, Asperger syndrome, Rett syndrome, fragile X syndrome, and PDD-NOS. Autism, Asperger syndrome, Rett syndrome and fragile X are all specifically described in the DSM-IV — the manual that practitioners use to diagnose neurological disorders.
Many children have some symptoms of one PDD and some symptoms of another, but not enough of any one of the four specific disorders to receive a diagnosis. Thus, they do have a PDD — but they do not have Rett syndrome, fragile X, Asperger syndrome, or autism. As a result, they receive the catch-all diagnosis of PDD-NOS.
There is a common belief that the diagnosis PDD-NOS means that a child has, in essence, a touch of autism. In fact, this may be true or untrue. A child may, for example, have only a few mild symptoms of a PDD and still qualify for the PDD-NOS label. On the other hand, he may have very severe delays in language and communication skills, but still not qualify for a specific autism diagnosis.
At present, physicians are not in agreement as to exactly when a child should be diagnosed with PDD-NOS, autism, or Asperger syndrome. As a result, it is very possible for the same child to receive different diagnoses from different physicians while exhibiting exactly the same symptoms.
Employment
The following are some examples of accommodations available to people with disabilities when taking pre-employment tests:
What is alternative format?
Alternative format is any format that is different from the existing test. Alternative format may be: large print, Braille, color-coded text, audio (reader, tape/cd, or computer).
What is extended time?
Extended time means allowing the test-taker extra time to complete the test. The amount of extended time should be correlated to the test-taker’s disability or limitations. Common examples of extended time include: time and a half, double time, and unlimited time.
What is a reader?
A reader is a person who reads the test to the test-taker. This person should be familiar with the terminology or language used on the test. A reader does not interpret, re-word, or explain the test. A reader reads the test directions, questions, and answer choices to the test-taker.
What is a scribe?
A scribe is a person who writes down, or otherwise records, the test-taker’s responses. The scribe does not create answers for the test-taker or help the test-taker identify correct answers. The scribe simply writes the test-taker’s answers down on the test or answer sheet.
What type of tests will people need accommodations for?
A person with a disability can ask for an accommodation on any exam. Some examples of exams are: teaching license exams, driver’s license exams, college entrance exams, exams in college or technical school, employment tests, and typing tests.
Who can ask for accommodations in testing?
Individuals with disabilities that inhibit their abilities to take tests can ask for an accommodation.
How does a person with disability ask for a testing accommodation?
A person with a disability can ask for an accommodation when registering to take a test. Oftentimes, the testing company provides testing accommodation forms to submit. The individual can also make a request verbally or in writing. The person with a disability is responsible for providing documentation of a disability, and the individual can describe the type of accommodation that will be effective.
Do testing accommodations cost the test-taker extra money?
No. The test-taker needing an accommodation pays the same cost as any person taking the same test.
Will test scores or standards be lowered/changed/altered for person with disability?
Generally, no. If all test-takers must obtain a certain “passing score,” so must the test-taker with a disability. The test-taker with a disability may need an accommodation to help meet the standard, but the standard does not have to be lowered, changed, or altered.
One exception to this rule is a situation where the test standard is arbitrary or is not related to the educational or employment requirements. For example, an employee must be able to type 40 words per minute to pass an employment test, but typing is not an essential function of the job.
Will a person with a disability be granted a “test exemption” as an accommodation?
Generally, no. If the test is a requirement of the application process, the job, class or program, or licensing credentials, the test-taker with a disability will probably have to take the test. The test-taker with a disability may, however, ask for an accommodation to assist with the taking the test.
Accommodations
Note: People with disabilities may experience limitations in cognitive abilities, motor abilities, and sensory abilities that can affect test-taking performance. People who have disabilities may have some or all of the limitations listed below. The degree of limitation will vary from individual to individual along with accommodation(s) provided.
Limitations in Cognitive/Neurological Abilities
Test-takers who may need the following accommodations include people with: TBI, MS, MR, fibromyalgia, LD, ADD or ADHD, cancer, and psychological impairments.
Memory: Test-takers may have difficulty remembering events or activities on the day of the test.
- Post or announce: reminders, location of the testing room, location of bathrooms, time remaining, materials to put away or to keep out during testing
- schedule one test per test day during test session
- allow extended time/flexibility (example: take math section on Saturday, reading section on Monday, and writing on Tuesday.)
Lack of Concentration or Organization: Test-takers may be distracted or disorganized when taking a test. Possible accommodations include:
- testing in a private room
- providing extended time
- providing a reader
- providing the test on tape
- reducing/eliminating distractions
- allowing breaks
- seating test-taker away from doors or windows, and other distractions
Time Management/Performing or Completing Tasks: Test-takers may be unable to complete or perform tasks in a timely manner or meet timelines. Possible accommodations include:
- testing in a private room
- providing extended time
- having proctor announce time in intervals
- using a clock or watch
- allowing test-taker to maintain written task-list
- allowing test-taker to use watch or timer programmed to alarm or vibrate at set intervals
Reading Print Material: Test-takers may be unable to read test materials. Possible accommodations include:
- providing a reader for the test-taker
- providing test on tape/CD-ROM
- providing extended time
- administering test in private room
- giving instructions in bold print
- allowing the use of a line guide or ruler to keep place in test book or answer sheet
- testing on computer with voice output
- using symbols or pictures where appropriate
- color-coding test by sections or subjects
- putting multiple choice in bold
Writing words, sentences, or paragraphs: Test-takers may be unable to construct written responses as required on the test. Potential accommodations include:
- allowing test-taker to write draft first
- providing a scribe
- allowing verbal responses instead of written responses
- allowing use of graphic organizer
- allowing use of scratch paper
- allowing use of dictionary or thesaurus
- allowing use of computer word processing to create written response: assisting with grammar, assisting with spelling, assisting with time management
Performing Mathematical Calculations: Test-takers may be unable to “do math” as required on the test. Possible accommodations include:
- allowing the use of a calculator (including talking calculator)
- allowing the use of other counting devices (fingers, toes, pencils, beans, etc.)
- allowing the use of written formulas
- allowing the use of scratch paper
- using flash cards
- allowing the use of times table list/multiplication chart
- allowing the use of pictures/graphics with word problems
Limitations in Motor Abilities
Test-takers who may need the following accommodations include people with TBI, MS, MD, fibromyalgia, paraplegia, quadriplegia, amputations, cancer, CP, back conditions, little people, and people who are obese.
Sitting: Test-takers may have difficulty sitting for long periods of time while taking a test. Test-takers may also have difficulty sitting in a traditional chair or desk. Possible accommodations include:
- providing space at table instead of desk
- allowing for frequent breaks
- providing extended time
- allowing test-taker to alternate sitting/standing
- using an alternative chair, cushion, or footrest
Writing: Test-takers may have difficulty physically writing responses or recording answers as required by the test. Possible accommodations include:
- using any writing product (not just a #2 pencil)
- allowing additional time
- allowing verbal response
- using a scribe
- providing writing aids
- allowing frequent breaks
- using a clipboard to hold paper while writing
- using line guide, writing template, or ruler
Turning Pages: Test-takers may have difficulty turning pages of the test booklet, or holding the test booklet open. Potential accommodations include:
- having a proctor turn pages
- providing page-turning devices
- providing reader(s)
- providing test on tape/CD
- unstapling booklet and laying flat
- using table instead of desk
Typing: Test-takers may have difficulty typing responses. Possible accommodations include:
- allowing practice on test device or unit
- using speech recognition
- using one handed-keyboards
- using alternative input devices: alternative keyboards and alternative mice
Limitations in Sensory Abilities
Test-takers who may need the following accommodations include people who are deaf or hearing impaired, blind or visually impaired, have TBIs, Expressive Language Disorders, or Auditory Processing Disorders.
Hearing: Test-takers may have difficulty hearing in the testing environment. Possible accommodations include:
- having proctor/administrator use microphone (FM loop)
- putting test-taker in private room
- putting test-taker in front of room
- facing student who reads lips
- posting time prompts in writing
- providing interpreter for sign-language
Seeing: Test-takers may have difficulty seeing the test or test materials, or other visuals in the testing environment. Potential accommodations include:
- announcing time prompts
- providing test on tape
- providing reader
- providing alternative format
- providing magnification
- allowing use of talking calculator
- providing test in alternate foreground or background colors
- using screen readers (voice output)
- allowing test-taker to get familiar with test environment
- allowing for use of assistance dog (care for animal during test time)
Communicating: Test-takers may have difficulty communicating in the testing environment. Possible accommodations include:
- providing interpreter for sign-language
- communicating in writing
- providing extended time
- communicating use of symbols instead of words
- communicating via auxiliary device such as
- speech board
- communication cards
- alpha-numeric pager
- TTY
Other Limitations
Panic Attacks: Test-takers may experience panic attacks during test administration. Test-takers who may need the following accommodations include people with ADD and psychological impairments. Possible accommodations include:
allowing frequent breaks
- extending time
- providing a private room
- providing a regular room – sit in back of room so test taker can leave if necessary
- allowing test-taker to become familiar with test environment
- allowing test-taker to choose own seat
- test administrators have plan of action to deal with emergencies such as
- passing out, having seizure, or conduct problems
Diarrhea/Vomiting/Nausea: Test-takers may have difficulty managing bodily functions. Test-takers who may need the following accommodations include people with psychological impairments, MS, MD, intestinal disorders, and cancer. Possible accommodations include:
- allowing frequent breaks
- providing extended time
- providing a private room
- providing regular room – sit in back of room so test-taker can leave discreetly
Headaches: Test-takers may experience mild to severe headaches during the testing administration. Test-takers who may need the following accommodations include people with migraines, vision impairments, and psychological impairments. Potential accommodations include:
- allowing frequent breaks
- allowing use of sunglasses or ball-cap
- turning off fluorescent lights if in private testing room
- using a glare guard
- using a flicker free computer monitor
Fatigue: Test-takers may experience mild to severe fatigue during the testing administration. Test-takers who may need the following accommodations include people with fibromyalgia, chronic fatigue syndrome, MS, and cancer. Possible accommodations include:
- allowing frequent breaks
- providing extended time
- providing private room
- scheduling one test per day on test day
- allowing extended time/flexibility
- providing space to lay down during breaks
Temperature Sensitivity: Test-taker may get hot or cold during testing administration. Test-takers who may need the following accommodations include people with fibromyalgia, cancer, MS, MD, and circulatory disorders. Possible accommodations include.
- allowing use of blanket or jacket
- adjusting temperature in room
- using a cool vest
- using a fan
- placing individual by window
- placing individual away from vent
- allowing test-taker to bring gloves, socks, etc.
Chemical Sensitivity: Test-takers may experience mild to severe reactions to chemicals, fragrances, or perfumes. Test-takers who may need the following accommodations include people with multiple chemical sensitivity, asthma, and migraine headaches. Potential accommodations include:
- having proctor wear no perfume
- testing in a private room
- placing individual by window
- having the individual use a mask
- using a fan
- providing HEPA filter in room – turn on prior to start of test
Dietary needs: Test-takers may need to eat, drink, or take medications during the test administration. Test-takers who may need the following accommodations include people with diabetes, cancer, intestinal disorders, and psychiatric impairments.
- providing extended time
- providing private room
- allowing test-taker to eat during test
- allowing test-taker to drink during test
- allowing time to administer medications to self
References
Many community-based organizations (like Asperger Manitoba Inc., Autism Society of Manitoba, St.Amant Centre, etc.) provide workshops on autism spectrum disorders or can connect an employer with someone who can provide the needed training.
All people have the right to reasonable accommodations in their lives, taking into account their needs, the ability of society to respond to those needs and the equivalent cost to doing so. If you are concerned about your rights to accommodation, speak to the human resources department at your workplace to learn more.
The Manitoba government states “Employers shall make reasonable accommodation for an individual’s special needs where those needs are associated with any characteristic protected by The Human Rights Code (Manitoba)”.
To learn more visit www.gov.mb.ca/csc/policyman/accomm.html
Manitoba Social Services and Programs
Health Sciences Centre- Child Development Clinic and Let’s Get Started Program: 204-787-2423
St.Amant Autism Programs: 204-256-4301 extension 3467
Autism Outreach Services – Through Children’s disability Services
MATC – Neurodevelopmental Disorder Program: 204-958-9660
*Children’s disability Services: http://www.gov.mb.ca/fs/pwd/css.html#content
*Community Living disability Services: http://www.gov.mb.ca/fs/pwd/supported_living.html#content
*marketAbilities Program: http://www.gov.mb.ca/jec/eia/marketAbilities/index.html
*Service Locations: Winnipeg Service Locations: www.gov.mb.ca/fs/misc/loc/winnipeg.html
Rural and Northern Service Locations:
Autism Society of Manitoba: info@autismmanitoba.ca
Asperger Manitoba Inc.: info@asperger-manitoba.ca
MFEAT: gmercier@mymts.net
Community Living Manitoba: aclmb@aclmb.ca 204-786-1607
A roadmap to services and supports has been developed to help guide families through the process. It can be viewed at http://www.stamant.ca/wp-content/uploads/2013/03/Road-Map-of-Services-October-2012.pdf
Children’s DisAbility Services (formerly known as Children’s Special Services (CSS)) can offer support to children and their families affected with a disability. A diagnosis of Asperger Syndrome allows your family to access these services. The supports available are listed on the government of Manitoba website: http://www.gov.mb.ca/fs/pwd/css_answers.html and include:
- Respite: respite can be either hired by Children’s DisAbility Services or you may find someone to provide your respite and be reimbursed each month for the services you paid to the support worker. The purpose of the respite can be twofold, to give the family a break from the high demand care that is often required when caring for a child with a disability and to give a child the chance to experience life in the community with an adult, other than the parent.
- Supplies and Equipment: not all supplies and equipment are covered. However, if a child is bed wetting, Children’s DisAbility Services can assist with the purchase of anti-bedwetting devices and/or pull-ups.
- Summer Gap Programming: This service can provide the funding for a support worker to attend a two week summer camp with your child, with the aim of helping your child to maintain or further improve skills gained during the previous school year.
You may self-refer to Children’s DisAbility Services or the professional that diagnosed your child can do the referral for you. If you are making the referral yourself, ensure that you have documentation of your child’s diagnosis, and contact you regional Family Services office. In Winnipeg, regional offices can be located through http://www.gov.mb.ca/fs/misc/loc/winnipeg.html. Outside of Winnipeg go to http://www.gov.mb.ca/fs/misc/loc/ruralnorthern.html. Depending on your location you name will be placed on a waiting list and a Children’s DisAbility Services worker will contact you to get further information regarding your child and the service needs of your family.
Community Living disABILITY Services (CLDS) (formerly the Supported Living Program) offers a range of day and residential services aimed at providing adults with a mental disability, defined as significantly impaired intellectual functioning existing concurrently with impaired adaptive behaviour and manifested prior to the age of 18 years, but excludes mental disability due exclusively to a mental disorder as defined in section 1 of The Mental Health Act. The program provides the opportunity for independence in a community setting to the extent possible for each individual. CLDS supports that are potentially available include residential services, day services and related support services. To learn more, contact you regional Family Services office. In Winnipeg, regional offices can be located through http://www.gov.mb.ca/fs/misc/loc/winnipeg.html. Outside of Winnipeg go to http://www.gov.mb.ca/fs/misc/loc/ruralnorthern.html.
The Employment and Income Assistance Program (EIA) provides financial help to Manitobans who have no other way to support themselves or their families. For people who are able to work, EIA will help them go back to work by providing supports to employment.
EIA provides benefits (money) to help you with the costs of things like:
- food, clothing, personal and household needs
- shelter and utilities (e.g. water, hydro, heat)
- basic dental, optical and prescription drugs
- health-related supplies or equipment not provided by other programs
- supports to help you find and start a job
EIA provides additional benefits to cover extra costs for people living in remote or northern regions of Manitoba.
You may be eligible for assistance if the total cost of your or your family’s monthly basic needs is more than your total financial resources. Your financial resources are based on your income and assets. Some of your income and assets may not affect your eligibility.
The amount of your or your family’s basic needs is based on:
- the number of people in your family, their ages and relationships to each other
- the EIA basic allowance rate for your family size
- the cost of your shelter, utilities and fuel
- the cost of some of your ongoing health needs
For information on how to apply for EIA or to set up a Pre-Intake Orientation, make an intake appointment, or find the EIA office that you should go to, please call
- 948-4000 if you are in Winnipeg
- 1-877-812-0014 (toll free) if you are outside of Winnipeg
Respite is a short-term, regular period to time set aside for parents to take a break from caregiving. Families can choose from a number of options, depending upon their circumstances and eligibility for supports.
- Office-administered respite, where a respite agency hires staff and matches available staff to family needs;
- Self-administered respite, where families receive funding (either through Children’s disability Services, Child and Family Services or Community Living disability Services) and hire their own respite staff;
- Facility-based respite, where families can work with a service provider that has a designated apartment or room where the child or adult can stay with a respite worker while the family takes a break.
The Government of Manitoba has compiled a series of fact sheets to help individuals with disabilities and their families access needed information across their lifespan. This can be found at www.gov.mb.ca/fs/imd.
Each fact sheet focuses on a theme and gives you information to help get you started on your journey to finding the right disability service for you and your family. The fact sheets provide links to additional resources as well as contact information should you wish to connect directly with a specific program, service or resource.
In Winnipeg, there is a mobile crisis response service available through the Winnipeg Regional Health Authority. You can learn more about it here.
Other supports include the following:
24-hour Crisis Lines:
| Service | Phone |
| Klinic Crisis Line | 204-786-86861-888-322-3019TTY 204-784-4097 |
| Manitoba Suicide Line | 1-877-435-7170 |
| Kids Help Phone | 1-800-668-6868 |
| Klinic Sexual Assault Crisis Line | 204-786-86311-888-292-7565TTY 204-784-4097 |
| Manitoba Farm and Rural Support Services | 1-866-367-3267 |
| Macdonald Youth Services | 204-949-47771-888-383-2776 |
Mental Health Services Contacts by region:
| Region | Intake Numbers |
| Winnipeg | 204-788-8330 (adult)204-958-9660 (child and adolescent) |
| Assiniboine | 204-571-2952 |
| Brandon | 204-578-2400 |
| Burntwood | 204-677-5350 |
| Central | 204-239-3000 (Portage area)204-325-0946 (Winkler area)1-888-310-4593 (for both) |
| Churchill | 204-675-8322 |
| Interlake | 204-785-7752 |
| Nor-Man | 204-687-1340 |
| North Eastman | 204-444-6147 |
| Parkland | 204-638-2103 |
| South Eastman | 204-346-7018 |
Preparing for the Future
It is important, as caregivers of children, youth and adults with ASD, to plan for the future. This may include planning living arrangements, caregiver succession, and wills and estate planning.
There are many Federal and Provincial Tax Credits and Programs aimed at easing the financial burden of raising a child with a disability or of living with a disability in Canada. These include:
The Primary Caregiver Tax Credit (Manitoba) http://www.gov.mb.ca/finance/tao/caregiver.html
The Disability Tax Credit (Canada) http://www.cra-arc.gc.ca/E/pbg/tf/t2201/README.html
The Canadian Child Tax Benefit (Canada) http://www.cra-arc.gc.ca/bnfts/cctb/menu-eng.html
The Registered Disability Savings Plan (Canada) http://www.servicecanada.gc.ca/eng/goc/rdsp.shtml
The Planned Lifetime Advocacy Network has created a useful and informative website on this topic: http://www.rdsp.com
To learn more about these and other financial planning tools, visit a trusted financial planner or accountant. , visit a trusted lawyer with experience working with families of children with disabilities.
People with disabilities have the same rights as any other citizen of Manitoba and Canada. In addition, you have the right to reasonable accommodations in your day to day life according to our Charter of Rights and Freedoms and as outlined in the United Nations Convention on the Rights of People with Disabilities.
Manitoba passed Accessibility Legislation in December 2013. Changes in how Manitoba society better accommodates people with disabilities will be emerging over the course of the ensuing years.
School Systems
Each post-secondary education institution offers an array of supports to students with disabilities. These can include preferred classroom seating, alternate testing environments, increased time to complete assignments and tests/exams, scribes for note-taking, voice recording for lectures, and much more.
You can learn more at http://www.neads.ca/en/norc/eag/eag_en.pdf or by visiting websites for the post-secondary education site you are attending or considering and contacting their disability services/accessibility services department.
Student-Specific Planning
Through a student-specific planning a student support team works to identify a student’s unique learning needs and to determine, implement and evaluate appropriate educational programming. A student’s Individual Education Plan (IEP) documents the student-specific planning in place that will help the student move the next step beyond their current level of performance. Information about this planning process can be found at http://www.edu.gov.mb.ca/k12/specedu/iep/index.html.
Special Needs Categorical Funding
Level 2 and 3 funding is part of the Special Needs Categorical support provided through the Funding of Schools Program. Categorical support is available for students with special needs who require and receive extensive supports based on a comprehensive educational needs assessment. Students who have moderate to severe ASD may be eligible.
Information about Student Services Funding can be viewed at http://www.edu.gov.mb.ca/k12/specedu/funding.html.
School Age Applied Behaviour Analysis (ABA) Services
The school age ABA program provides consultation and training for 20-25 hours per week of ABA in school for three years or up to the end of grade 4, whichever comes first. To be part of the school-age ABA program students must have participated in a preschool ABA program and have a reliable diagnosis of one of the following: Autism Disorder, Asperger’s Syndrome, Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) or Autism Spectrum Disorder. A child’s guardians are asked to discuss the inclusion of ABA in their child’s programming with their school.
More information about the school-age ABA program can be found at
http://www.stamant.mb.ca/main/ABAProgram.html.
Behaviour Analyst Autism Consultation Service (BAACS)
This St Amant service provides and the student support team of students who have completed the school-age ABA program with consultative services and workshop training in ABA learning principles.
For more information about this St. Amant service, call
204-256-4301.
The Interdivisional Program for Students with Autism (IPSA)
Manitoba Education in partnership with the Winnipeg School Division and Louis Riel
School Division support four specialized classroom settings (two middle years programs and two senior years programs) for students with severe to profound ASD. Referral information is shared with school division Student Services Administrators when vacant spaces become available.
Transition from School to Community
Transition planning should begin in the school year in which the student enters high school. The process concludes in June of the calendar year in which the student turns 21 or when he/she graduates. During this time, professionals, the student, his/her support network and others work together to provide the student with a co-ordinated transition from school to life in the community.
Bridging to Adulthood: a Protocol for Transitioning from School to Community can be found at http://www.edu.gov.mb.ca/k12/docs/policy/transition/index.html.
Supports for Educators Working with Children who have ASD
Supporting Inclusive Schools: A Handbook for Developing and Implementing Programming for Students with Autism Spectrum Disorder This support document is intended to be a planning and programming resource for school teams who support students with ASD. The “ASD Handbook” includes information on planning for the student with ASD as well as evidence based teaching and instructional strategies. Appendices include tools and forms and additional topics to assist the school team in developing and implementing appropriate educational programming for their student with ASD
A PDF version of the document can be viewed at: http://www.edu.gov.mb.ca/k12/specedu/aut/index.html
Print copies of the document (Stock #80498) can be ordered from the Manitoba Text Book Bureau at http://www.mtbb.mb.ca/catalogue/en/.
Directory of Services
A directory listing organizations within Manitoba that may be of support to students, families and school teams programming for students with Autism Spectrum Disorder can be found on the ASD Handbook website at:
http://www.edu.gov.mb.ca/k12/specedu/aut/index.html.
Online Professional Learning – Developing and Implementing Programming for Students with ASD
Educators may participate in a 20 contact hour online professional learning experience delivered by Manitoba Education. The course is designed to lead educators through the process of planning appropriate education programming for students with ASD.
Information about this learning opportunity is shared with school division Student
Services Administrators annually. For more information contact Brent Epp, Consultant for Student Services – 204- 945-6885
Programming Consultation and Professional Development
The Student Services Unit of Manitoba Education can provide a school with direct consultative support for the planning and implementation of programming for students with exceptional needs including ASD. Professional development opportunities can also be arranged.
For more information contact Brent Epp, Consultant for Student Services – 204-945-6885
Manitoba Adolescent Treatment Centre (MATC) Neurodevelopmental Services Neurodevelopmental Services can provide educators with consultative support in programming for children with ASD and complex multi-diagnostic issues.
Schools throughout Manitoba can request this service through MATC centralized intake at 204-958-9660
Instructional Resources Library
The Instructional Resources Library provides Manitoba Kindergarten through Grade 12 educators with curriculum implementation support, educational research and professional development materials. The Instructional Resources Unit loans a variety of resources to Manitoba educators. Items can be requested in person, by phone, mail, fax or electronic mail. The collection includes many titles on ASD.
Circulation Desk, Instructional Resources Unit
1181 Portage Avenue
Winnipeg, Manitoba R3G 0T3
Telephone: 945-5371 or 800-282-8069, ext. 5371
In the school system, the classroom teacher is your first point of contact. More assistance may be found with the principal or vice principal and the school’s resource teacher. Further information may be found at the school division level with the student services administrator. At the Department of Education level, there is an autism consultant who can be contacted at 204-945-6885 or by emailing brent.epp@gov.mb.ca.
Support Groups
There are a number of support groups across the province, either autism spectrum disorder specific or with a cross-disability membership. You may find one near you by searching online, visiting the website for one of the autism spectrum disorders community organizations, or asking your community services worker. The data base within this webportal allows you to search for supports within various regions of the province.
There are a number of support groups across the province, either autism spectrum disorder specific or with a cross-disability membership. You may find one near you by searching online, visiting the website for one of the autism spectrum disorders community organizations, or asking your community services worker. The data base within this webportal allows you to search for supports within various regions of the province.
There are a number of support groups across the province, either autism spectrum disorder specific or with a cross-disability membership. You may find one near you by searching online, visiting the website for one of the autism spectrum disorders community organizations, or asking your community services worker. The data base within this webportal allows you to search for supports within various regions of the province.
There are a number of support groups across the province, either autism spectrum disorder specific or with a cross-disability membership. You may find one near you by searching online, visiting the website for one of the autism spectrum disorders community organizations, or asking your community services worker. The data base within this webportal allows you to search for supports within various regions of the province.
There are a number of support groups across the province, either autism spectrum disorder specific or with a cross-disability membership. You may find one near you by searching online, visiting the website for one of the autism spectrum disorders community organizations, or asking your community services worker. The data base within this webportal allows you to search for supports within various regions of the province.
Therapy Options
There are many people offering educational and medical solutions for kids with autism. Sometimes the variety and the conflicting claims can be overwhelming.
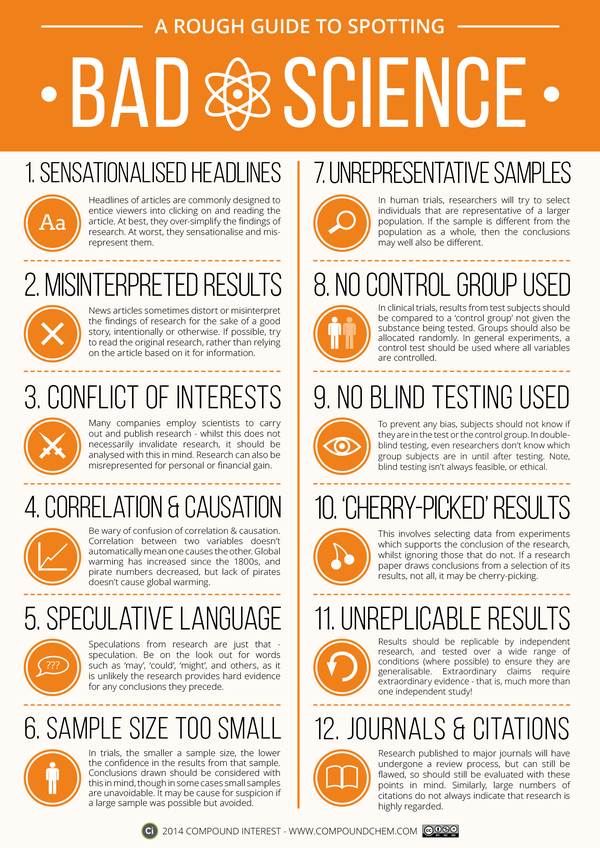
“Research-based” is a term that can be used inappropriately.
This infographic is a place to start for people wanting to understand how to recognize good research.
Source: http://www.iflscience.com/chemistry/tips-spotting-bad-science
Adults can benefit from many of the same approaches to providing support as seen in children. Many benefit from learning skills in a way that allows them to generalize their learning and not tie the learning to one specific environment. To learn more about the different types of therapies used with individuals who have ASD, visit our “Therapy Options” page.
Particular areas of focus include skills for independent living/living with independence, pre-employment and employment-readiness skills, job-coaching, mentorship, and social skill training.
This is an emerging field among many service providers.
Types of Treatments
There are many different types of treatments available. For example, auditory training, discrete trial training, vitamin therapy, anti-yeast therapy, facilitated communication, music therapy, occupational therapy, physical therapy, and sensory integration.
The different types of treatments can generally be broken down into the following categories:
- Behavior and Communication Approaches (such as ABA, RDI, DIR/Floortime, TEACCH, Sensory Integration, etc)
- Medication
- Complementary and Alternative Medicine
Please visit our “Therapy Options” page for detailed information on the types of therapies used with children who have ASD.
Importance of early intervention
Research shows that early intervention treatment services can greatly improve a child’s development. Early intervention services help children from birth to 3 years old (36 months) learn important skills. Services include therapy to help the child talk, walk, and interact with others. Therefore, it is important to talk to your child’s doctor as soon as possible if you think your child has an ASD or other developmental problem.
Even if your child has not been diagnosed with an ASD, he or she may be eligible for early intervention treatment services. In addition, treatment for particular symptoms, such as speech therapy for language delays, often does not need to wait for a formal ASD diagnosis. While early intervention is extremely important, intervention at any age can be helpful.
An evidence-based treatment approach for people with an ASD is called applied behavior analysis (ABA). ABA is an evidence based approach, widely accepted among health care professionals and used in many schools and treatment clinics. ABA is a way of changing behavior and helping children to learn. It encourages positive behaviors and discourages negative behaviors in order to improve a variety of skills.
St. Amant
St. Amant directs the Manitoba ABA Program for Children with Autism (MABACA). It is funded by the provincial government and provides intensive ABA treatment for children with autism between the ages of 2 to 6 y. Each child in the program receives 35 hours of therapy per week, including 27 hours with a tutor, three hours with a senior tutor, and five hours with a parent, all supervised by a clinical consultant.
St. Amant is also developing more flexible approaches to the use of ABA for those unable to commit to this level of intensity, and also helps with the transition into child care and school settings.
DIR/Floortime is a developmental approach to supporting the learning of children with autism. There is emerging evidence of its effectiveness as an intervention for children with ASD. It’s based on the idea that engaging interactions between parents and caregivers are the key to fostering growth through the social and development stages that all children experience. Social and emotional development are foundational to all areas of learning, and so as children progress in emotional regulation, communication and the ability to connect socially, they are able learn in other ways as well. DIR takes into account each child’s unique learning profile, and teaches parents how to use that information to engage and support their child.
Occupational therapists help people participate in the things they want and need to do through the therapeutic use of everyday activities (occupations). Occupational therapy teaches skills or provides alternate strategies that help the person live as independently as possible. Skills might include dressing, eating, bathing, managing emotions, making plans, and relating to people.
When an injury, illness, disability or other problem limits a persons ability to:
• Take care of himself or herself,
• Participate in learning or paid or unpaid work, or
• Enjoy leisure time, e.g. hobbies, sports, spending time with family,
then they may want to learn some new skills from an occupational therapist.
Occupational therapists will often work with individuals who have ASD to help in areas like supporting early childhood development, creating schedules, providing strategies and treatments for daily functioning, or using sensory integration therapy.
This video provides an excellent explanation along with examples of how an occupational therapist can help people achieve their goals.
Relationship Development Intervention (RDI) takes the perspective that a key feature of autism is severe learning disabilities that strongly impact a person’s quality of life. These difficulties can be described as a lack of ability to make decisions in a complex, always changing environment. The ability to think flexibly and to learn from one’s own experience and those of others requires flexible and sophisticated levels of thinking.
Because of poor neural integration, children with ASD tend to think in much more rigid terms. They may excel at gathering information about certain topics, but have difficulty applying information in real life situations.
RDI works directly with parents to teach them how to guide their children through everyday experiences in order to expand their ability to work with changing circumstances, solve problems, and learn new skills.
You can read more about RDI on the RDI Connect website.
There are many health care professionals who work with individuals who have autism spectrum disorder (ASD) using sensory integration therapy. Many people who have ASD are overly sensitive to certain sounds, touches, smells, movement and sights. Individuals with ASD may enjoy a particular sense, and seek out that sensation seemingly to the exclusion of everything else. (e.g. watching spinning fans, listening to the same story or part of a story over and over, avoiding music or other sounds, walking on tip toe to avoid placing their whole foot on the floor, etc.)
Sensory integration therapy helps the person deal with different types of sensory information that are causing problems in their daily life. This type of approach is a un-established treatment.
Speech language therapy helps to improve a person’s communication skills. Some people are able to learn verbal communication skills. For others, using gestures or picture boards is more realistic. Because some individuals with ASD have difficulty communicating with others, they may have to see a speech language pathologist.
TEACCH originated in North Carolina in 1971. It works to understand of the effects of autism on individuals, to promote meaningful engagement in activities, flexibility, independence, and self-efficacy. A common strategy TEAACH uses is visual cues to teach skills. For example, picture cards can help teach a child how to get dressed by breaking information down into small steps.